What is Ankylosing Spondylitis?
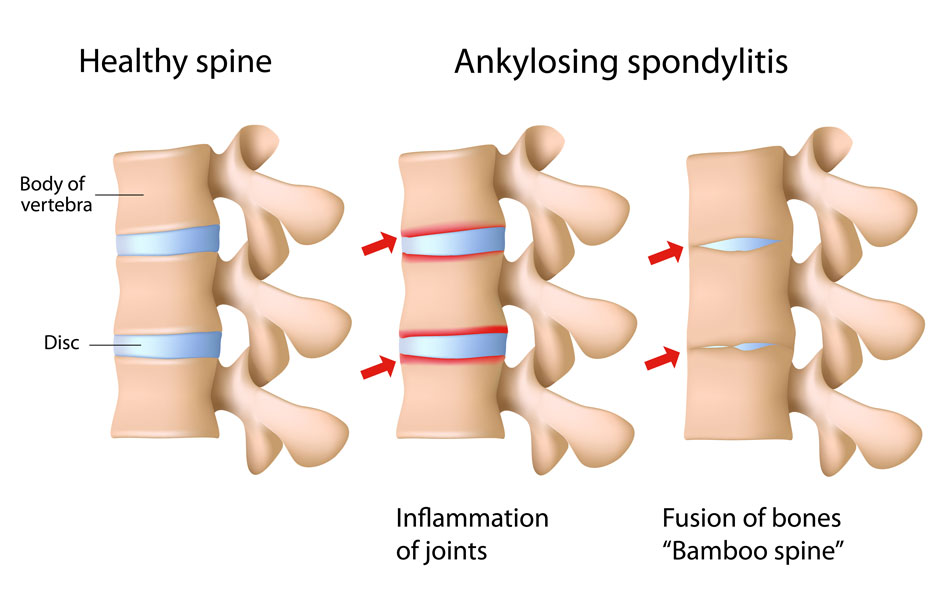
Ankylosing spondylitis is a form of ongoing joint inflammation (chronic inflammatory arthritis) that primarily affects the spine. This condition is characterized by back pain and stiffness that typically appear in adolescence or early adulthood. Over time, back movement gradually becomes limited as the bones of the spine (vertebrae) fuse together. This progressive bony fusion is called ankylosis.
The earliest symptoms of ankylosing spondylitis result from inflammation of the joints between the pelvic bones (the ilia) and the base of the spine (the sacrum). These joints are called sacroiliac joints, and inflammation of these joints is known as sacroiliitis. The inflammation gradually spreads to the joints between the vertebrae, causing a condition called spondylitis. Ankylosing spondylitis can involve other joints as well, including the shoulders, hips, and, less often, the knees. As the disease progresses, it can affect the joints between the spine and ribs, restricting movement of the chest and making it difficult to breathe deeply. People with advanced disease are also more prone to fractures of the vertebrae.
Causes of Ankylosing Spondylitis
Ankylosing spondylitis is likely caused by a combination of genetic and environmental factors, most of which have not been identified. However, researchers have found variations in several genes that influence the risk of developing this disorder.
Variations in several additional genes have also been associated with ankylosing spondylitis. Although these genes play critical roles in the immune system, it is unclear how variations in these genes affect a person’s risk of developing ankylosing spondylitis. Changes in genes that have not yet been identified are also believed to affect the chances of developing ankylosing spondylitis and influence the progression of the disorder. Some of these genes likely play a role in the immune system, while others may have different functions. Researchers are working to identify these genes and clarify their role in ankylosing spondylitis.
Diagnosis
A rheumatologist is commonly the type of physician who will diagnose ankylosing spondylitis (AS), since they are doctors who are specially trained in diagnosing and treating disorders that affect the joints, muscles, tendons, ligaments, connective tissue, and bones. A thorough physical exam, including X-rays, individual medical history, and a family history of AS, as well as blood work (including a test for HLA-B27) are factors in making a diagnosis.
Ankylosing Spondylitis Treatments
Currently, there is no known cure for AS, but there are treatments and medications available to reduce symptoms and manage pain. Recent studies show that the newer biologic medications can potentially slow disease progression in some people. Note that different people respond to different medications with varying levels of effectiveness. Thus, it may take time to find the most effective course of treatment.
